In recent discussions surrounding the health risks associated with substance abuse, experts have highlighted the profound effects of drugs and alcohol exposure on children, particularly during critical stages of pregnancy.
“The impact of drugs and alcohol on children, particularly during pregnancy, is devastating and often irreversible. Exposure can lead to a range of effects from mild to severe,” said Barbra Sagoe, a doctor in Family Medicine & Pediatrics at Parkview Health.
Infants exposed to drugs while in utero face serious health challenges. One of the significant issues they may experience is Neonatal Abstinence Syndrome (NAS). This condition arises due to the withdrawal effects from substances that the mother used during pregnancy.
“NAS is really just the medical way to say that they have symptoms of drug withdrawal after delivery,” said traveling NICU nurse Meredith Rethlake.
The vulnerability of the developing fetus is particularly pronounced during the early stages of pregnancy. This period is critical for proper development and growth. Any adverse factors can have significant implications for the fetus’s health.
“Early pregnancy is especially critical as major organs and structures are being formed, making the fetus highly vulnerable. Disruptions to processes like blood supply, cell division and cell metabolism can cause significant structural defects, DNA damage, and altered cell migration, impacting organ development and function,” said Sagoe.
As the discussion on the critical nature of early pregnancy progresses, it’s essential to recognize the profound impact that substance exposure can have on newborns. The signs of withdrawal in infants, often referred to as Neonatal Abstinence Syndrome (NAS), reveal the severity of this issue.
“Withdraw in babies looks very similar to withdraw in adults. NAS infants can be irritable and difficult to console, jittery, run fevers, be poor feeders, have frequent vomiting and diarrhea which often causes awful diaper rash, and in severe cases, babies can even have seizures,” Rethlake said.
Every year, more than 20,000 babies are born in the United States dependent on illegal or prescription drugs, resulting in a troubling condition known as neonatal abstinence syndrome (NAS) according to Nichq.org
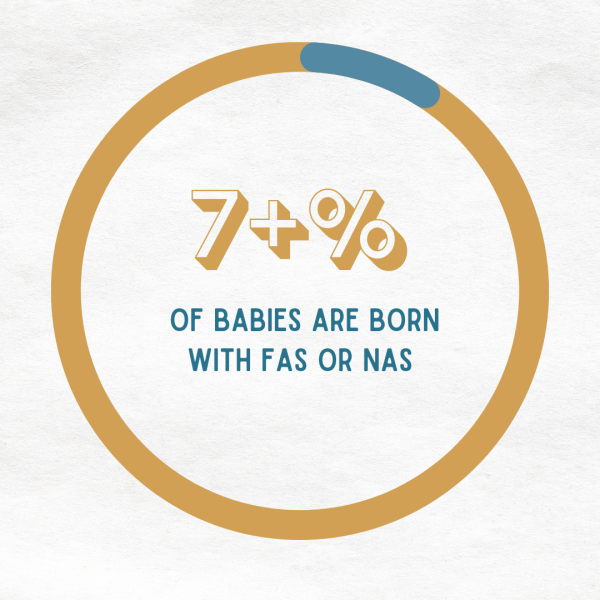
Given that the total number of births annually is approximately 3,667,758, according to National Center for Health Statistics these statistics underscore a significant public health issue that affects not only the newborns but also their families and communities.
“The illicit substances that I have seen the most frequently include marijuana/THC, heroin, fentanyl, and methamphetamine.I’ve frequently seen babies whose mother was in a treatment program and being prescribed methadone or buprenorphine to help prevent withdraw symptoms after choosing to stop using illicit opiates”, Said Rethlake. “The ones that always surprise me are the babies who experience withdraw from their mom’s antidepressants, anti anxiety medications, or seizure medications.”
Maternal substance use during pregnancy can lead to a range of physical health problems in infants, varying from very mild, barely noticeable effects to significant complications. The impact of different substances can differ widely, leading to various outcomes for the baby.
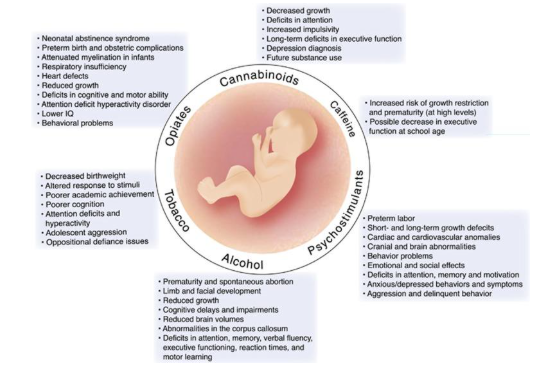 As experts continue to examine the effects of in utero drug exposure, the range of consequences becomes increasingly clear.
As experts continue to examine the effects of in utero drug exposure, the range of consequences becomes increasingly clear.
“This can range from very mild barely noticeable effect to significant complications,” said Sagoe.
These complications highlight the intricate interplay of neurotransmitters during development. This complexity is crucial for understanding various developmental processes.
The implications of in utero drug exposure extend beyond immediate health concerns, significantly influencing mental health and cognitive development throughout a child’s life.
“In utero drug exposure impacts serotonin and dopamine, both of which play a role in mood, emotional regulation, and the reward system of our brains. With dysregulation of these neurotransmitters, you can have a variety of mental health issues including anxiety, depression, and ADHD,” said Rethlake.
This disruption is not merely a temporary issue that will resolve itself over time. Instead, it has the potential to create ongoing challenges that can affect various aspects of our daily lives and operations. Therefore, it is essential to address the root causes and implement effective strategies to mitigate its long-term impacts.
“Prenatal exposure to substances like alcohol, cocaine, opiates, marijuana, and tobacco can lead to significant lifelong cognitive and behavioral challenges, including deficits in attention, memory, and executive functioning,” said Sagoe. “Children affected may display issues such as hyperactivity, anxiety, and increased risk of behavioral disorders. These impairments can persist into adolescence and adulthood, impacting academic performance and increasing the likelihood of substance use disorders.”
The decline in smoking among pregnant women is a notable public health achievement, reflected in recent data indicating a significant decrease in births to mothers who smoke.
According to the Centers for Disease Control and Prevention, there was a 41% decline from 2016 to 2021, including a 16% drop from 2020 to 2021. This downward trend suggests successful public health interventions and increased awareness of the risks associated with smoking during pregnancy. 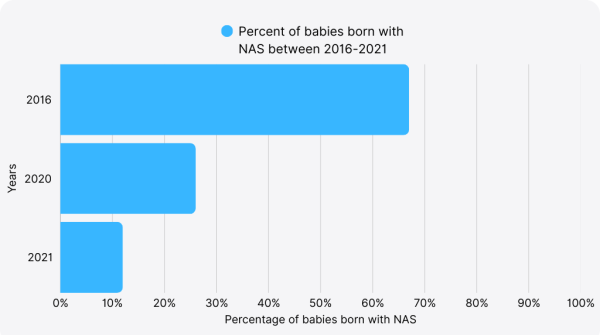
The detrimental effects of smoking on both the mother and the developing fetus are well documented. Smoking during pregnancy increases the risk of preterm birth, low birth weight, and birth defects. It can lead to long-term health problems for the child, including respiratory issues, learning disabilities, and sudden infant death syndrome. The reduction in smoking rates among pregnant women is a positive sign for the health of future generations.
Another critical indicator of maternal and infant health is the rate of Neonatal Abstinence Syndrome (NAS), a condition where newborns experience withdrawal symptoms due to exposure to addictive substances in the womb. Encouragingly, between 2016 and 2020, 28 states experienced a decline in NAS births, with 23 of those states reporting a substantial 10–30% decrease.
This positive trend suggests that ongoing efforts to promote healthier pregnancies are beginning to yield results. However, experts emphasize that this decline should serve as a vital reminder of the necessity for early intervention and comprehensive support systems for expectant mothers.
Healthcare professionals are advocating for the prioritization of thorough prenatal care, which can greatly improve outcomes for both mothers and their infants. By investing in resources such as counseling, education, and community support networks, that are addressing the multifaceted challenges that pregnant women encounter today.
Ensuring that every expectant mother has access to these essential services is crucial for fostering a healthier future generation. While celebrating this progress, it is imperative that we continue to focus on enhancing support to sustain and build upon these improvements in maternal health.
“Early recognition or pregnancy and initiation of prenatal care allows for more options with regards to the pregnancy, at which point the pregnant mother can discuss the risks with their OB. Additionally, any program that offers assistance for people struggling with substance use should be able to provide information on the dangers of substance use,” said Rethlake.
Early intervention is crucial not only for the health of the mother but also for the developing fetus. This proactive approach underscores the need for comprehensive educational programs that target women of childbearing age, creating a culture of awareness that addresses substance use long before pregnancy occurs.
By fostering open dialogues about the risks associated with alcohol and drugs, we can empower individuals to make informed choices, ultimately leading to healthier outcomes for families and communities.
“To prevent anything starts with education and awareness,” said Sagoe. “Health workers and educators have been and should continue to inform the public, particularly women of childbearing age about the dangers of alcohol and drug use even before pregnancy, emphasizing that there are no safe levels of use.”
The issue of Neonatal Abstinence Syndrome (NAS) can be effectively addressed through a combination of strategic interventions aimed at prevention.
As highlighted by the CDC Clinic, “strategies to prevent the incidence of NAS center on responsible opioid prescribing and access to preconception care and family planning services.”
This emphasizes the critical role that healthcare providers play in managing opioid prescriptions while simultaneously ensuring that women have the necessary resources to plan their pregnancies effectively.
The CDC Clinic supports this approach by stating that “another primary prevention strategy that might reduce the incidence of NAS is ensuring access to family planning and preconception care for women who use opioids.”
These strategies underscore the importance of comprehensive care in reducing the prevalence of NAS among newborns affected by maternal opioid use.
Neonatal Abstinence Syndrome (NAS) represents a significant yet often overlooked consequence of the opioid epidemic gripping communities across the nation. Over the past decade, the incidence of NAS has surged dramatically, marking a troubling trend that corresponds with rising rates of opioid prescriptions and usage among pregnant women.
This increase in NAS cases not only impairs the health and development of affected infants but also burdens the healthcare system with substantial financial costs related to extended hospital stays and specialized care.
To effectively mitigate the incidence of NAS, it is essential to implement responsible opioid prescribing practices. This includes the rigorous use of Prescription Drug Monitoring Programs (PDMPs), which help providers identify potentially unsafe prescribing patterns and prevent misuse.
Enhancing accessibility to preconception health services can play a critical role in advising and supporting women of childbearing age in managing their health, thus reducing the risk of opioid exposure during pregnancy.
Access to comprehensive treatment programs for maternal opioid use disorder is also crucial. Such interventions not only support mothers in overcoming addiction but also promote healthier outcomes for their infants.
Standardized treatment protocols for infants diagnosed with NAS are equally important, as they ensure that affected newborns receive consistent and effective care that can reduce withdrawal symptoms and long-term developmental issues.
By focusing on these primary prevention strategies and improving access to necessary treatments, we can significantly diminish the impact of NAS and foster better health outcomes for both mothers and their children.